Garden snails and slugs that could be lethal.

The rat lungworm (Nematoda), Angiostrongylus
cantonensis.
For three weeks a 10-month old baby girl fought for life after having contracted rat lungworm
from an infected slug, most probably from crawling
across its slime trail or eating a slug.
"Doctors told us....., her
whole brain stem was destroyed and she would be a
vegetable for the rest of her life." and the family
made the heart-breaking decision to switch off her
life support.
NSW Health said it was aware of two recent cases of
rat lungworm in northern Sydney. Source: The Sunday Telegraph October 16, 2011 Sydney Australia.
 Select an article on this page.
Select an article on this page.
1: Introduction:
2: The rat lungworm cycle.
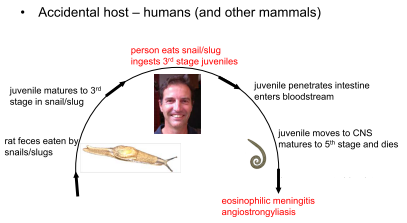
3: The rat lungworm infection.
4: Human Eosinophilic Meningitis.
5: How is it prevented?
Introduction.
Human angiostrongyliasis is an infection caused
by a nematode parasite of rats. The tiny parasitic
roundworm Angiostrongulus cantonensis (pronounced
an-gee-o-stron-guh-luss can-tun-en-sis) is commonly
called the rat lungworm.
The mature, adult form of the
nematode is found only in rats.
The rat lungworm (Nematoda), Angiostrongylus
cantonensis, causes neurological disease in humans and
several fatalities have occurred in Australia (see review in
Prociv et al. 2000).
It is of increasing concern due to the
continuing expansion of its geographical range which
now encompasses much of Southeast Asia, Melanesia,
Polynesia, eastern Australia, parts of Africa, India, the
Caribbean and the south-eastern United States of
America (USA).(2)
Naturally occurring, non-human infections were first
recognised in dogs in Brisbane in 1972 and in Sydney in 1989 and 1991
(Collins et al 1992).
In the city of Brisbane, the first human infections probably occurred in 1959.
From the 1970s, increasing numbers of autochthonous infections have been reported
along the central east coast of the continent (southeast Queensland and northern New South Wales),
involving humans, rats, dogs, horses, flying foxes and marsupials.
In 1989 the parasite was
discovered in Sydney, almost 1,000 km to the south, in dogs. In that city,
it has since been diagnosed as a cause of neurological disease in increasing numbers of dogs,
flying foxes, marsupials and zoo primates.
Presumably, these infections resulted from the
ingestion of snails or slugs, and it seems that virtually all species of native and exotic
terrestrial molluscs can serve as intermediate hosts.
The first reported case of human angiostrongyliasis ( rat lungworm infection )
acquired in Sydney in 2001.
It is not known how the parasite was introduced to this continent,
or how it has spread over such an extensive territory, although eventually its range could
encompass the entire east coast, and potentially other regions. " (2)

World distribution map of recorded human Angiostrongylus cantonensis infections(3)
 A wide spectrum of snails and semi-
slugs (Gastropoda), including the African giant land
snail, Achatina fulica, serve as intermediate hosts of the
lungworm and it may occur also in a range of paratenic
hosts. As a consequence, the route of infection in human
cases varies geographically.
A wide spectrum of snails and semi-
slugs (Gastropoda), including the African giant land
snail, Achatina fulica, serve as intermediate hosts of the
lungworm and it may occur also in a range of paratenic
hosts. As a consequence, the route of infection in human
cases varies geographically.
In Asia and Australia, most
cases are probably acquired by ingesting raw intermediate hosts, snails, slugs or
planarians either directly or on fresh vegetables that have not
been thoroughly washed.
For example, by eating a small baby slug on a lettuce leaf.
According to University of Hawaii snail researcher Rob Cowie, it is when people touch or
eat raw snails or slugs or their "slime trails" that the threat to human health occurs. (4)
Slugs and snails can be clear and less than a centimetre long, making
them hard to spot, but each one can carry thousands of worms.
The rat lungworm cycle.
The rat lungworm. (5)
 Rats eating snails or slugs
ingest "third stage" worms or parasites that penetrate through the intestine to the bloodstream.
The parasites then reach the central nervous system of the rat, reaching the "fifth stage" or young
adulthood.
They mature in the bloodstream and mate in the rat's heart and pulmonary artery.
The female parasite lays eggs that hatch into "first stage" worms that are expelled in the
rat faeces and then eaten by slugs or snails.
Rats eating snails or slugs
ingest "third stage" worms or parasites that penetrate through the intestine to the bloodstream.
The parasites then reach the central nervous system of the rat, reaching the "fifth stage" or young
adulthood.
They mature in the bloodstream and mate in the rat's heart and pulmonary artery.
The female parasite lays eggs that hatch into "first stage" worms that are expelled in the
rat faeces and then eaten by slugs or snails.
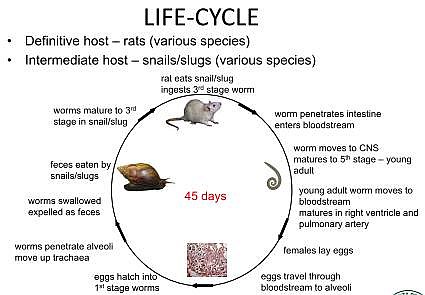
The rat lungworm life cycle images courtesy of Rob Cowie(4)
The rat lungworm infection.
First reported case of human angiostrongyliasis ( rat lungworm infection ) acquired in Sydney in 2001.
A Sydney-based man ate two garden slugs Limax maximus, the leopard slug, an
intermediate host for Angiostrongylus cantonensis
as a dare during a party narrowly
escaped death from a rare form of meningitis, an often fatal swelling around the brain.
As well as developing meningitis - inflammation of the membrane
that surrounds the spine and the brain - the man developed encephalitis - swelling
of the brain and spinal cord.
"He nearly died - his consciousness was impaired and he was very ill
indeed in hospital. He had extremely high pressure inside his head,"
Dr.Pryor told ABC Science Online.
While the Sydney man survived, others have not been so lucky. In an earlier case, a
young child in subtropical Brisbane died, believed to have eaten slugs crawling on milk bottles
which had been left at the front door. Another man had acquired the disease during a holiday in Fiji.
However, the risk of dying from ingesting the parasites was "low".
One reason for the low risk is that the natural host for the parasite is the rat, and so
if the parasite finds itself inside a human it tends to die off after a couple of weeks or so.
"So you don't have to treat the disease - it cures itself when the organism dies, when it
discovers you're not a rat."
"He had a lot of the organisms actually invade the brain," says Dr.
Pryor of the Sydney man.
Source: Man's brain infected by eating slugs
- ABC Western Queensland - Australian Broadcasting Corporation
http://www.abc.net.au/science/articles/2003/10/20/969551.htm Accessed: 22/12/2011
Source: MJA 2003; 179 (8): 430-431
Accessed: 22/12/2011.
Symtoms and Human Eosinophilic Meningitis.
Angiostrongylus cantonensis,
also known as Parastrongylus cantonensis, is the commonest infectious cause of
eosinophilic meningitis worldwide.
Angiostrongylus meningitis is usually mild and resolves spontaneously over 6 weeks.
Occasionally, cases are severe and may have chronic sequelae and death may incurr. (6)
Severe Eosinophilic meningitis.
The immune reaction caused by the dead worms results in serious
inflammation and damage in the nervous system and brain, and can lead to
symptoms including headache, stiff neck, numbness, tingling or pain in the
skin, fever, nausea and vomiting, blurred vision, weakness, joint pain and
neurological abnormalities. More severe symptoms can include paralysis of the
legs, bowel and bladder dysfunction, seizures, coma and, although rare, death. (6)
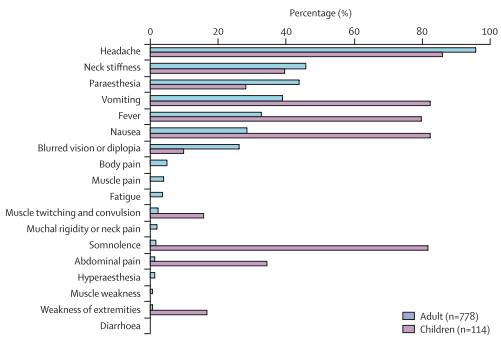
References reported in Thailand, Taiwan, mainland China, and the USA (6)
How is it prevented?
Factsheet - NSW Health
• Don't eat raw snails or slugs. If eating snails, ensure they are thoroughly cooked first.
• Supervise infants and young children in environments where they may find snails and slugs.
• Wash fresh vegetables and lettuces well before eating in case they have snails or slugs (or their slime) on them.
• Wash your hands well after gardening or handling snails or slugs.
• Consider controlling snails and slugs around vegetable patches and gardens and control vermin
around the home. If snail pellets or rodent baits are used it is very important that precautions are taken
to ensure young children don't accidentally eat them.
Source: Factsheet - NSW Health http://www.health.nsw.gov.au/factsheets/infectious/rat_lung_worm.html
 Other Articles at this site.
Other Articles at this site.
1: Flesh-eating bacteria in Australia.
2: Lethal ants in Australia.
3: Chronology of Australian Major Bush fires.
4: Chronology of Australian Major Droughts.
5: Early Settlers' Homes and Bush Huts in Australia.
6: Early Settlers in Victoria Australia.
7: Is there a risk of a volcanic eruption in Australia ?
References and other Sources:
Source:(1) Image of slug Limax maximus and garden snail ( Helix aspersa ) courtesy of CSIRO, Gastropoda:
(2) The spread of Angiostrongylus cantonensis in Australia. Southeast Asian J Trop Med Public Health. 2001;32 Suppl 2:126-8.
[PubMed - indexed for MEDLINE] http://www.ncbi.nlm.nih.gov/pubmed/12041575
Accessed: 22/12/2013
Source:(3) One Health Newsletter Volume 4 Issue 1 Winter 2011 http://www.onehealthinitiative.com
Source:(4) Robert H. Cowie Pacific Biosciences Research Center, University of Hawaii,
Honolulu, Hawaii Biology: taxonomy,identification, and life cycle of Angiostrongylus cantonensis.
RAT LUNG WORM DISEASE SCIENTIFIC WORKSHOP
HONOLULU, HAWAII AUGUST 16 - 18, 2011
Accessed: 2/1/2013
Source:(5) Image courtesy of (4)
Source:(6) Human angiostrongyliasis Qiao-Ping Wang, De-Hua Lai, Xing-Quan Zhu,
Xiao-Guang Chen, Zhao-Rong Lun www.thelancet.com/infection Vol 8 October 2008 Accessed: 22/12/2013
Further Reading:
• Gutteridge BH, Bhaibulaya M, Findlater C. Human larval meningitis possibly following lettuce ingestion in Brisbane. Pathology 1972; 4: 63-64.
• Mason KV: Haematological and cerebrospinal fluid findings in canine neural angiostrongylosis.
Australian Veterinary Journal 66:152-154, 1989
• Prociv P, Carlisle MS. The spread of Angiostrongylus cantonensis in Australia. Southeast Asian J Trop Med Public Health. 2001;32 Suppl 2:126-8.
• Sanjaya N Senanayake, Don S Pryor, John Walker and Pam Konecny MJA 2003; 179 (8): 430-431
• Yang F: Observation on the cats and a dog infected by Angiostrongylus cantonensis
[Parastrongylus cantonensis]. Chinese Journal of Zoonoses 15, 1999
Rat lungworm. ( 7 pages )
by Romsey Australia is licensed under a Creative Commons Attribution 2.5 Australia License.


Revised 03/01/2012