Worldwide increases in foodborne illness
Food Poisoning in Australia:
 Number of cases of food poisoning in Australia 5.4 million yearly.
Number of cases of food poisoning in Australia 5.4 million yearly.
Number of new daily cases of food poisoning in Australia 11,500.
120 People die due to food poisoning each year in Australia.
Source: Food Standards Australia and New Zealand accessed 15-08-2009
The most common pathogens responsible for foodborne
gastroenteritis were pathogenic E. coli, norovirus, Campylobacter and non-typhoidal
Salmonella.
According to the " Foodborne illness in Australia " (3) publication,
contaminated food was estimated to cause about 6,000 cases
of illnesses other than gastroenteritis in Australia each year, where,
Toxoplasmosis was estimated to be the most common non-gastroenteritis illness,
causing 5,900 new symptomatic illnesses each year. Some serious illnesses, such as invasive listeriosis, where 20% of infections are fatal were also attributed to contaminated food.
Contaminated food was also estimated to cause about 42,000
episodes of sequelae following acute gastroenteritis, each year where, the most common illness was
reactive arthritis, responsible for an estimated 21,000 episodes, while irritable bowel
syndrome was responsible for 20,200 episodes each year.(3)
Source: Foodborne illness in Australia Annual incidence circa 2000 Australian Government Department of Health and Ageing Document: foodborne_report.pdf Accessed 15-11-2009
Worldwide increases in foodborne illness
Surveillance and monitoring by a number of countries indicates that foodborne illness is increasing around the world.
In Australia, notification rates for both campylobacteriosis and salmonellosis (common foodborne illnesses) have continued to increase annually.
![]() Select an article on this page.
Select an article on this page.
#: Latest News relating to Food Poisoning.
1: Changes in food production
2: Our changing eating habits and fast food.
3: New and emerging pathogens
4: Fried rice and Bacillus cereus.
5: Red Kidney Bean , Kinkoti Bean Poisoning .
6: Honey Poisoning (tutu toxin , Grayanotoxin )
7: Fungus in our Food. ( Mycotoxins )
8: Histamine Fish Poisoning (HFP)
9: Ciguatera Fish Poisoning.
10: Other potential problems with seafood.
11: Bottled Mineral Water.
12: Our Drinking Water.
13: Latest Updates relating to Food Poisoning.
14: Latest Australian and Worldwide Food Recalls.
15: List of Food Poisoning Causes and Symptoms
16: Human health and Genetically Modified foods
17: Australia fourth in world food safety rankings
18: Deliberate Food Adulteration - Lethal Food
19: Hotel serves ice-cream laced with human excrement
20: Meat that Glows in the Dark - Photobacteria
21: Name and Shame food premises in N.S.W.
Changes in food production
In developed countries such as Australia, there have been a number of structural changes in the food supply system.
These include intense farming practices, more extensive food distribution systems and the increasing move towards minimally processed food.
If potential hazards associated with these practices are not recognised and controlled, they can contribute to an increased risk of foodborne illness.
Extensive food distribution systems
There is a trend, both in Australia and internationally towards wider geographic distribution of food from large centralised processors.
This increases the potential for rapid, widespread distribution of contaminated product.
In 1985, 185,000 people in Chicago contracted salmonellosis from contaminated pasteurised milk distributed by one dairy plant.
In one outbreak in 1994, over 200,000 people across the United States contracted salmonellosis from contaminated icecream made in Minnesota and distributed nationally.
Industry consolidation and mass distribution of foods increase the risk that breakdowns in food safety will cause further widespread outbreaks of foodborne disease.
Outbreaks can be difficult to detect as the increase in cases may not be apparent against the background level of illness (Tauxe 1997). Often it is a fortuitous concentration of cases in one location or the identification of an unusual strain that leads to the identification of a widespread outbreak.
Our changing eating habits
Around sixty to eighty per cent of foodborne illness arises from the food service industry.
Fast food restaurants and salad bars, rare 50 years ago, are today a primary source of food consumption for many Australians.
It is estimated that the number of food service outlets in Australia, has grown 57 per cent with Australians spending 30 per cent of their food budget on take away food and dining out .
Food Standards Australia New Zealand Incidence of Food Borne Illness
In Australia, New Zealand, the United States and the United Kingdom, around 60 per cent to 80 per cent of foodborne illness arises from the food service sector (Crerar et al 1996; Auckland Healthcare 1998; Bryan 1980; Cowden at al 1995; Todd 1985).
New and emerging pathogens
Three of the four most significant foodborne pathogens,
Campylobacter, Listeria and enterohaemorrhagic E. coli (EHEC),
were unrecognised as causes of foodborne illness 20 years ago (United States General Accounting Office 1996).
Campylobacter jejuni was first identified as a human pathogen in 1973 and is now the most commonly reported bacterial cause of foodborne illness in the United States .
Unlike other foodborne pathogens, C. jejuniis often associated with sporadic infections and can lead to long-term effects including reactive arthritis and Guillain-Barré syndrome.
Handling raw poultry and eating undercooked poultry have been identified as major risk factors for contracting campylobacteriosis.
Infection with Escherichia coli serotype O157:H7 (E. coli) was first described in 1982. Subsequently, it has emerged rapidly as a major cause of bloody diarrhoea and acute renal failure. The infection is sometimes fatal, particularly in children. Outbreaks of infection, generally associated with beef, have been reported in Australia, Canada, Japan, United States, in various European countries, and in southern Africa. Outbreaks have also implicated alfalfa sprouts, unpasteurized fruit juice, lettuce, game meat and cheese curd.
In 1996, an outbreak of Escherichia coli O157:H7 in Japan affected over 6,300 school children and resulted in 2 deaths. This is the largest outbreak ever recorded for this pathogen.
Listeria monocytogenes (Lm) is considered emerging because the role of food in its transmission has
only recently been recognized.
In pregnant women, infections with Lm can cause abortion and stillbirth, and in infants and
persons with a weakened immune system it may lead to septicemia (blood poisoning) and meningitis.
The disease is most often associated with consumption of foods such as soft cheese and processed
meat products that are kept refrigerated for a long time because Lm can grow at low temperatures.
Outbreaks of listeriosis have been reported from many countries, including Australia, Switzerland,
France and the United States.
Outbreaks of Listeria monocytogenes in France in 2000 and in the USA in 1999 were caused by contaminated pork tongue and hot dogs respectively.
Foodborne trematodes are also emerging as a serious public health problem, especially
in south-east Asia but also in Latin America, in part due to a combination of increased aquaculture
production, often under unsanitary conditions, and of consumption of raw and lightly processed fresh
water fish and fishery products.
Foodborne trematodes can cause acute liver disease, and may lead to
liver cancer. An estimated 40 million people world wide are affected.
Source: World Health Organization Fact sheet N°124
Although there is an increasing incidence of foodborne illness, only a small proportion of food poisoning cases are formally reported (Hennessey et al 1996; Crerar et al 1996; Kaferstein 1997; United States General Accounting Office 1996).
The Foodborne Diseases Active Surveillance Network (FoodNet) was established in the United States in 1995 to provide better data on the incidence of foodborne illness (United States Department of Health and Human Services 1998).
FoodNet undertakes active surveillance for foodborne diseases and related epidemiological studies and currently covers 6 per cent of the United States population.
Reference: Food Standards Australia New Zealand Incidence of Food Borne Illness 2007
FOODNET Data shows seven years of Failure. 2008
The U.S. Centers for Disease Control report on foodborne illness rates for seven
pathogens in 2007 looks depressingly like the reports for the last six years.
Food contaminated with disease-causing bacteria are still causing 76 million cases of food poisoming in
the U.S. each year, sending 325,000 Americans to the hospital and killing 5,000, mostly
young children, the elderly and those with chronic illnesses.
Last
year the CDC acknowledged that there has been virtually no change in the rate of
Campylobacter since 2001.
Source: Consumer Federation of America April 11, 2008
CDC, Preliminary FoodNet Data on the Incidence of Infection with Pathogens Transmitted Commonly
Through Foods—10 States, 2007, Mortality and Morbidity Weekly Report, April 11, 2008.
Fried rice and Bacillus cereus.
Incidences of rice-associated food poisoning have been linked to the practice of preparing bulk rice in advance, in anticipation of subsequent need.
Fried rice is a leading cause of Bacillus cereus emetic-type food poisoning in Australia. B. cereus is frequently present in uncooked rice, and heat-resistant spores may survive cooking.
If cooked rice is subsequently held at room temperature, surviving spores will germinate into vegetative forms.
The vegetative forms will multiply, these forms may then produce a heat-stable toxin and this low molecular weight toxin can survive brief heating, such as stir frying.
There are two illness associated with B. cereus, emetic and diarrhoeal illness.
The emetic illness is caused by the ingestion of a heat-stable toxin produced by the microorganisms in the food.
The diarrhoeal illness is caused by the ingestion of moderate to high number of B. cereus and their subsequent production of toxin in the stomach.
Symptoms:
The emetic type of food poisoning, with symptoms similar to that caused by Staphylococcus aureus, is characterised by nausea and vomiting.
The symptoms of B. cereus diarrhoeal illness, similar to Clostridium perfringens food poisoning, include watery diarrhoea, abdominal cramps, and pain.
Nausea may sometimes occur, and vomiting rarely occurs.
Onset times for the emetic illness is usually ½ to 6 hours after consumption of contaminated foods.
For the diarrhoeal illness onset times are usually 6 to 15 hours.
The emetic illness usually lasts less than 24 hours, while the diarrhoeal illness usually persist for 24 hours in most instances.
Source A.C.T Health 2006 www.health.act.gov.au Reference. http://www.safefood.net.au/
Bacillus cereus
B. cereus food poisoning is the general description, although two recognized types of illness are caused by two distinct metabolites.
The diarrheal type of illness is caused by a large molecular weight protein, while the vomiting (emetic) type of illness is believed to be caused by a low molecular weight, heat-stable peptide
Associated Foods:
A wide variety of foods including meats, milk, vegetables, and fish have been associated with the diarrheal type food poisoning.
The vomiting-type outbreaks have generally been associated with rice products; however, other starchy foods such as potato, pasta and cheese products have also been implicated.
Food mixtures such as sauces, puddings, soups, casseroles, pastries, and salads have frequently been incriminated in food poisoning outbreaks.
Melbourne, Vic: Food poisoning outbreak 27/03/2002
Contaminated rice is believed to be the cause of severe food poisoning that hit more than 250 people celebrating the Islamic New Year in Melbourne's northern suburbs.
Health authorities tested samples of the suspect rice and other food served at the festival after 10 hospitals and medical centres were flooded with violently ill people.
Initial tests on rice dishes indicated the likely bacterial germ was bacillus cereus
The outbreak was the worst mass food poisoning in Victoria since 1997 when more than 550 people fell ill after eating pork rolls infected with salmonella.
Source: EMERGENCY MANAGEMENT AUSTRALIA,
Lectin In Undercooked Red Beans And Rice Causes Food Poisoning
Lectins, a family of proteins believed to be a natural insecticide that is abundant in undercooked legumes and grains, can cause food poisoning.
Red Kidney Bean Poisoning
Is caused by a toxic agent, Phytohaemagglutnin (Kidney Bean Lectin).
This toxic agent is found in many species of beans, but it is in highest concentration in red kidney beans (Phaseolus vulgaris).
The unit of toxin measure is the hemagglutinating unit (hau).
Raw kidney beans contain from 20,000 to 70,000 hau, while fully cooked beans contain from 200 to 400 hau.
White kidney beans, another variety of Phaseolus vulgaris, contain about one-third the amount of toxin as the red variety; broad beans (Vicia faba) contain 5 to 10% the amount that red kidney beans contain.
Symptoms
As few as 4 or 5 beans can bring on symptoms.
Onset of symptoms varies from between 1 to 3 hours and is usually marked by extreme nausea, followed by vomiting, which may be very severe.
Diarrhea develops somewhat later (from one to a few hours), and some persons report abdominal pain and have been hospitalized, but recovery is usually rapid (3 - 4 hours after onset of symptoms) and spontaneous.
" .. ingestion of lectin has also been linked to colorectal cancer and celiac disease, a common problem in which individuals are sensitive to gluten, a mixture of proteins derived from wheat flour that includes lectins.
The small intestine of the celiac sufferer is unable to properly absorb nutrients after gluten ingestion. "
Source: Dr. Paul L. McNeil, Medical College of Georgia, U.S. 4-Aug-07
http://www.accessibility.com.au/news/
The syndrome
is usually caused by the ingestion of raw, soaked kidney beans, either alone or in salads or casseroles.
Several outbreaks have been associated with "slow cookers" or crock pots, or in casseroles which had not reached a high enough internal temperature to destroy the glycoprotein lectin.
It has been shown that heating to 80 degrees C. may potentiate the toxicity five-fold, so that these beans are more toxic than if eaten raw.
In studies of casseroles cooked in slow cookers, internal temperatures often did not exceed 75 degrees Celsius.
Source FDA (U.S. Food and Drug Administration) Center for Food Safety & Applied Nutrition Reference. Bad Bug Book (Foodborne Pathogenic Microorganisms and Natural Toxins Handbook).
NOTE: To render kidney, and other, beans safe for consumption:
* Soak in water for at least 5 hours.
* Pour away the water.
* Boil briskly in fresh water for at least 10 minutes.
* Undercooked beans may be more toxic than raw beans.
This procedure has been recommended by the PHLS (Public Health Laboratory Services, Colindale, U.K.)
Tutu toxin in honey.
Tutin, a picrotoxin, is a naturally occurring toxin found in honey.
The toxin is produced as a result of bees gathering honeydew secreted by bugs feeding on sap of the poisonous ‘tutu’ plant (Coriaria arborea).
The toxin has no effect on bees and honeydew honey is chemically very similar to floral honey and cannot be distinguished by taste, sight or smell from other non-toxic honeys.
It cannot be degraded by any heating or processing of honey. The toxins are believed to be very stable, and poisoning cases have resulted from people eating honey that was several years old.
Comb honey poses a greater risk because it is eaten directly off the comb, increasing the chance of consuming honey with a high concentration of tutin.
Tutu is widely distributed throughout New Zealand, particularly along stream banks and in regenerating native scrub.
It historically occurs primarily in the Coromandel Peninsula, Eastern Bay of Plenty (EBOP) and the Marlborough Sounds, although it is possible it could occur elsewhere. Test results from the honey incident in March 2008 confirmed that the suspected tutu toxins and its derivative hyenanchin, were present in comb honey from the Coromandel Peninsula.
March 2008. New Zealand
22 People were poisoned after eating comb honey contaminated with tutin and its derivative hyenanchin.
Exposure to honey containing this naturally occurring toxin can produce symptoms such as vomiting, delirium, giddiness, increased excitability, or in more severe cases stupor, coma and violent convulsions.
It is generally accepted that as little as one teaspoon (approximately 10 ml) of unblended honey can have a severe effect on the human nervous system.
Prior to the March 2008 incident, the last recorded case from commercial honey was in 1974 involving 13 patients. There have been nine cases since 1974 with the last known poisoning occurring in 1991 in the EBOP area. Two poisonings have been caused by comb honey produced by hobby beekeepers in the Marlborough Sounds in 1982 and 1983 and the highest levels of tutin ever measured in honey were produced in this area.
Source: http://www.foodstandards.gov.au/newsroom/foodsurveillancenewsletter/winter2008.cfm
Honey Intoxication.
Honey intoxication is caused by the consumption of honey produced from the nectar of rhododendrons. The grayanotoxins cause the intoxication.
The specific grayanotoxins vary with the plant species.
These compounds are diterpenes, polyhydroxylated cyclic hydrocarbons that do not contain nitrogen.
Other names associated with the disease is rhododendron poisoning, mad honey intoxication or grayanotoxin poisoning.
Symptoms.
The intoxication is rarely fatal and generally lasts for no more than 24 hours.
Generally the disease induces dizziness, weakness, excessive perspiration, nausea, and vomiting shortly after the toxic honey is ingested.
Other symptoms that can occur are low blood pressure or shock, bradyarrhythima (slowness of the heart beat associated with an irregularity in the heart rhythm), sinus bradycardia (a slow sinus rhythm, with a heart rate less than 60), nodal rhythm (pertaining to a node, particularly the atrioventricular node), Wolff-Parkinson-White syndrome (anomalous atrioventricular excitation) and complete atrioventricular block.
In severe intoxication, loss of coordination and progressive muscular weakness result.
Several cases of grayanotoxin poisonings in humans have been documented in the 1980s. These reports come from Turkey and Austria.
The Austrian case resulted from the consumption of honey that was brought back from a visit to Turkey.
From 1984 to 1986, 16 patients were treated for honey intoxication in Turkey. The symptoms started approximately 1 h after 50 g of honey was consumed. In an average of 24 h, all of the patients recovered..
The Austrian case shows that with increased travel throughout the world, the risk of grayanotoxin poisoning is possible outside the areas of Ericaceae-dominated vegetation, namely, Turkey, Japan, Brazil, United States, Nepal, and British Columbia.
Source: Bad Bug Book (Foodborne Pathogenic Microorganisms and Natural Toxins Handbook).
Fungus in our Food. ( Mycotoxins )
Mycotoxins are toxic chemical products formed by mould species including
Penicillium, Aspergillus and Fusarium.
These moulds can
readily colonise food crops such as cereal grains, nuts and fruits, either in
the field or post harvest.
Consumption of foods produced from these commodities
poses a potential risk to human health because the toxins are resistant to
various food processes, including heat treatment.
Mycotoxins rarely cause acute
illness in developed countries, but long term consumption of low levels has been
linked to disease.
The mycotoxins of concern to the international food industry are:
| Mycotoxin | Of main concern | Potential health effect |
| Patulin | Fruit juices, particularly apple | Genetic mutations |
| Ochratoxin A | Cereals, wine, coffee | Kidney disease |
| Zearalenone | Cereals | Endocrine system disruption |
| Aflatoxins | Peanuts, tree nuts and maize | Liver cancer |
| Trichothecenes | Cereals | Acute vomiting/ diarrhoea (high dose required) |
| Fumonisins | Maize | Kidney and liver disease |
As harvest conditions in Australia are predominantly warm and dry, the threat of mycotoxin production in cereals is much lower here than in most other regions.
Contamination of Australian peanut crops by aflatoxins is an ongoing issue
however, particularly when plants become drought stressed in seasons when there
is low rainfall preceding harvest.
Source: Food Safety and Hygiene, November 2006 http://www.foodscience.com.au/fshbull/fshbull43a.htm
Ochratoxin.
Ochratoxin is present in a large variety of foods because it is produced by several fungal strains of the Penicillium and Aspergillus species that have varied physiologies and ecologies.
Ochratoxin is considered to be nephrotoxic, teratogenic, and immunotoxic, and
has been classified by the IARC as a Class 2B carcinogen, probable
human carcinogen.
Ochratoxin A, themaintoxin in this group, is found in wheat, corn,
and oats having fungal infection and in cheese and meat products
of animals consuming ochratoxin-contaminated grains (Aish and
others 2004).
A. ochraceus is found on dry foods such as dried and
smoked fish, soybeans, garbanzo beans, nuts, and dried fruit.
A. carbonarius is the major pathogen in grapes and grape product including
raisins, wines, and wine vinegars.
Although reported to occur in foods around the world, the main regions of concern are Europe
and, for some foods, Africa.
The Joint Expert Committee on Food
Additives of the Food and Agriculture Organization of the United
Nations and theWorld Health Organization (JECFA 2001) presented
data indicating that cereals, wine, grape juice, coffee, and pork are
the major sources of human ochratoxin exposure, at levels of 58%,
21%, 7%, 5%, and 3% of total ochratoxin intake, respectively.
Levels reported range from 100 to 700 ng/kg in cereals, 30 to 9000 ng/L
in European wines, 170 to 1300 ng/kg in coffee, and 150 to 2900
ng/kg in pork (Sage and others 2004).
Ochratoxin presence in European
wines is a relatively recent concern, with red wines typically
containing higher ochratoxin levels than rose or white wines.
Because of the large variety of food matrices in which ochratoxin
has been found, there is no universally suitable method of analysis.
Carcinogenic Toxins.
" The greatest human health concern related to mycotoxins is the cancer risk
based on long-term, low-level exposure to carcinogenic toxins such as the aflatoxins,
ochratoxin A, fumonisins, and zearalenone. "
" In some regions of Africa (Transkei), Asia (China), and Europe (Italy) the exposure
to fumonisins from maize is connected with higher incidence of oesophageal
cancer. "
Source: Peraica M, Domijan A-M. MYCOTOXINS IN FOOD AND HUMAN HEALTH
Arh Hig Rada Toksikol 2001;52:pp. 23–35
Deoxynivalenol contamination.
Another mycotoxin of contemporary relevance is Deoxynivalenol produced in
wheat, maize, and barley.
It is found frequently in US,
Canadian, European and Chinese wheat mostly associated
with cool, wet growing and harvest seasons that favour
the formation of scabs caused by Fusarium graminearum.
Outbreaks had been reported from India, China and the
USA. While the outbreaks in India and China occurred
among the general population the outbreak in the USA
had occurred in children in 17 schools in seven states who
had consumed burritos as part of the school lunch programme.
During that period, heavy contamination of deoxynivalenol
was reported in wheat in several states in the
USA. Deoxynivalenol toxicosis symptoms include nausea,
vomiting and pain in the abdomen. No mortalities were
reported.
Source: Source: Asia Pac J Clin Nutr 2008;17(S1):91-94
Human health problems associated with current
agricultural food production
Secretary General, Federation of Asian Nutrition Societies, Centre for Science, Society and Culture M 11,
Kakateeyanagar, Habshiguda, Hyderabad, India.
Recombinant DNA technology and genetically modified
foods.
" Risk to human health from Genetically Modified
(GM) foods is mainly related to toxicity, allergenicity and
antibiotic resistance.
The risk of toxicity may be directly
related to the nature of the product whose synthesis is
controlled by the transgene or the changes in metabolism
and composition that result from the gene transfer.
Most
of the toxicity risks can be assessed using scientific methods.
The introduction of newer proteins in transgenic
crops from organisms, which have not been consumed in
foods before, have the potential to become allergens.
Health risk assessment of genetically modified organisms
(GMOs) cultivated for food or feed is widely debated
throughout the world, and very little data have been published
on mid- or long-term toxicological studies with
mammals.
StarLink maize was genetically engineered by Aventis
Crop Science to express an insecticidal Bt derived protein
Cry9C.
The US Environmental Protection Agency (EPA)
had approved the registration of StarLink maize for restricted
use as animal feed and not for human consumption,
due to the presence of certain allergenic properties.
The Centre for Disease Control in the USA found that 28
persons had experienced allergic reactions after the ingestion
of taco shells made by Kraft foods that were found to
have traces of Starlink maize.
This resulted in a huge recall
of the product from the market by the US Food and
Drug Administration (FDA).
This example clearly indicate
the possibility of health concerns arising from certain
GM food events which were hastily approved "
Source: Asia Pac J Clin Nutr 2008;17(S1):91-94
Human health problems associated with current
agricultural food production
Secretary General, Federation of Asian Nutrition Societies, Centre for Science, Society and Culture M 11,
Kakateeyanagar, Habshiguda, Hyderabad, India.
NEW FOOD SCANDAL ROCKS THE USA
SAFEWAY BRAND CONTAINS ILLEGAL GM MAIZE
http://www.gene.ch/genet/2000/Oct/msg00016.html
Histamine Fish Poisoning (HFP)
Eating fish with high levels of histamine can result in histamine fish poisoning (HFP).
HFP was previously also called Scombroid Fish Poisoning.
Histamines in fish can cause allergic reactions in people ranging from
mild skin discomfort to nausea, vomiting and diarrhoea.
The level of histamine in fish, canned, frozen or fresh is affected by the presence of certain
proteins which are converted to allergenic products by bacteria present. Correct temperature
control can limit the production of histamines.
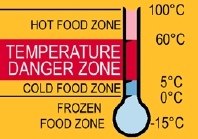 Fish are a particular concern when it comes to maintaining temperatures of less than 5ºC.
Fish are a particular concern when it comes to maintaining temperatures of less than 5ºC.
This
is because if the fish contain an amino acid called Histidine, the bacteria can turn this into
Histamine which is a physiological amine responsible for many allergic reactions.
Once histamine is formed it is not destroyed by freezing, cooking, smoking, curing or canning
This is the same histamine that causes problems for some people when high levels are produced in
cheese and red wine.
Histamine eaten in spoiled fish appears to be more toxic than an equal amount of histamine
taken orally in a solution. It is thought that the other biogenic amines (Putrescine, Cadaverine ) produced in fish may potentiate the histamine action.
The symptoms of Fish Poisoning ( HFP ) can be very similar to a severe allergic reaction, and can happen within
minutes to hours after ingestion of the toxic fish and may include:
· A burning/tingling sensation in/around the mouth.
· Rash and/or swelling over the chest and /or neck.
· Lowering of blood pressure.
· Headache.
· Itchy skin.
· Nausea.
· Vomiting.
· Diarrhoea.
Most of these symptoms will stop after a few hours.
Tuna and mackerel, members of the family Scombroidae tend to have high levels of histidine and are therefore more likely to be implicated in allergic reactions.
However, many non-scombroid species, for example sardines, blue fish, mahi mahi have caused HFP, so the term Scombroid Fish Poisoning is a misnomer.
The key to controlling histamine production is rapid cooling of the fish once caught and maintaining a temperature of less than 5ºC until it is cooked.
Best practice is to prevent amine production in the first place.
Source A.C.T Health 2006 www.health.act.gov.au
Ciguatera fish poisoning.
Ciguatera fish poisoning is caused by the consumption of fish contaminated by naturally occurring toxins produced by the algal dinoflagellate Gambierdiscus toxicus associated with coral reefs.
Ciguatoxin, which accumulates through the food chain, is thermostable and is not destroyed by cooking, freezing or other fish-processing methods. It does not affect the taste or texture of the fish. In humans, ciguatoxin produces gastrointestinal and characteristic neurological symptoms, consisting mainly of sensory disturbances
Ciguatera fish poisoning is widespread, affecting mainly tropical and sub-tropical areas of the world.
Most reported outbreaks in Australia have involved Spanish mackerel, but numerous other species of fish, including red bass, the chinaman and coral trout, have been implicated
An outbreak of 30 cases of ciguatera fish poisoning in outer Melbourne in September 1997 was traced to a 16.2 kg Maori Wrasse fish imported into Victoria from Trunk Reef in Queensland.
Symptom |
Number of cases | |
|---|---|---|
| n = 30 | % | |
Gastrointestinal |
||
| Diarrhoea | 20 |
67 |
| Abdominal Pain | 14 |
47 |
| Nausea | 9 |
30 |
| Vomiting | 5 |
17 |
Neurological |
||
| Paraesthesia of hands | 26 |
87 |
| Paraesthesia of feet | 23 |
77 |
| Hot/cold temperature reversal | 19 |
63 |
| Circumoral paraesthesia | 17 |
57 |
| Ataxia | 11 |
37 |
| Tremors | 7 |
23 |
| Dental pain | 4 |
13 |
Others |
||
| Myalgia | 23 |
77 |
| Weakness | 21 |
70 |
| Chills | 21 |
70 |
| Arthralgia | 17 |
57 |
| Neck Stiffness | 10 |
33 |
| Pruritis | 8 |
27 |
| Shortness of breath | 4 |
13 |
| Dysuria | 3 |
10 |
The incubation period ranged from 2 to 27 hours (median 8 hours). Symptoms varied in severity
Source: Communicable Diseases Intelligence Volume 24, No 11, November 2000. http://www.health.gov.au/
Other potential problems with seafood.
Nematode Anisakis: which infects marine animals.
Common in a broad range of fish in Northern and
Southern Southern hemispheres.
Humans become incidental hosts by consuming raw or undercooked seafood.
Allergic reactions occur in patients sensitised to allergens in
Anisakis these include anaphylaxis or acute urticaria,
when infected fish is eaten.
Recently described as a cause of anaphylaxis and other acute allergic reactions after eating fish,in regular fish eaters.
Most reports are from Spain and Japan.
Viruses
Hepatitis A, rotavirus, Norwalk virus group.
(noroviruses)
| Causative agent | Incubation period | Duration of illness | Predominant symptoms | Foods commonly implicated |
|---|---|---|---|---|
| Viruses | ||||
| Norovirus (and other caliciviruses) | 24-48 hrs | 12–60 hrs | Nausea, vomiting, abdominal cramping, diarrhea, fever, myalgia, and some headache. Diarrhea is more prevalent in adults and vomiting is more prevalent in children. | Oysters, clams, foods contaminated by infected food handlers, ready-to-eat foods salads, sandwiches, ice, cookies, fruit and untreated water contaminated by human faeces. |
| Rotaviruses | 24-72 hrs | Up to 7 days | Malaise, headache, fever, vomiting, diarrhoea | Foods contaminated by infected food handlers and untreated water contaminated by human faeces |
| Hepatitis A | 15-50 days | usually 1-2 weeks | Fever, nausea, abdominal discomfort, possibly jaundice | Shellfish, foods contaminated by infected food handlers and untreated water contaminated by human faeces |
| Other viral agents (astroviruses, adenoviruses, parvoviruses) | 10-70 hrs | 2-9 days | Nausea, vomiting, diarrhea, malaise, abdominal pain, headache, fever. | Fecally contaminated foods. Ready-to-eat foods touched by infected food workers. Some shellfish. |
Toxic shellfish poisoning.
Toxins from algae eaten by shellfish, diarrhoeic , paralytic, neurotoxic
and amnesic types.
| Causative agent | Incubation period | Duration of illness | Predominant symptoms | Foods commonly implicated |
|---|---|---|---|---|
| Shellfish toxins | ||||
| Paralytic shellfish poisoning (PSP) | Minutes to several hours | Several days | Burning and tingling around the mouth and extremities, nausea dizziness, potentially muscle and respiratory paralysis | Bivalve molluscs |
| Diarrhetic shellfish | 30 mins – 2 hrs | Hours to 3 days | Diarrhoea, nausea, vomiting. | Mussels, scallops and clams |
Source: Wharton DA, Hassal M –L, Aalders O. New Zealand Journal of Marine and Freshwater Research, 1999, Vol. 33: 643-648 Source: http://www.health.vic.gov.au/ideas/bluebook/food_water
Bottled Mineral Water
Bottled water could account for 12 per cent of infections by the bacterium campylobacter jejuni, the biggest cause of food-borne infection in the western world, say scientists.
As many as 6,000 of the 50,000 cases reported in England and Wales each year may be due to the bacterium, which causes stomach pains and diarrhoea, but in rare cases can prove fatal.
Contaminated water supplies, milk and poultry are recognised risk factors for campylobacter jejuni.
New research shows that bottled mineral water and non-lettuce salad vegetables such as tomato and cucumber are also potential hazards.
Bottled water was found to account for 12 per cent of the cases studied, salad 21 per cent and chicken 31 per cent.
Reference: Article Published in the American journal Emerging Infectious Diseases by Dr Meirion Evans, University of Wales in Cardiff. 2003
The Independent, (London), Oct 3, 2003 by John von Radowitz
Cases of the top two food poisoning germs (salmonella and campylobacter) are set to soar to more than 120,000 in just three months this summer according to the Food Standards Agency (FSA) U.K.
9 June 2008 http://www.food.gov.uk/news/pressreleases/2008/jun/germwatch
Our Drinking Water
Protozoan parasites such as Cryptosporidia and Giardia lamblia, and viruses like hepatitis A and E, rotavirus, Norovirus, poliovirus and echovirus can be present in drinking water even when the water is chlorinated.
People can become extremely sick by swallowing a few protozoa since they rapidly reproduce once inside a host organism.
Cryptosporidium caused a cryptosporidiosis outbreak in Milwaukee in 1993 that resulted in over 400,000 cases of serious illness and 100 deaths.
Emerging Issues in Water and Infectious Disease, World Health Organization, 2003
Britain orders Tests for drugs in drinking water supply. 29 September 2008
" Drinking water supplies are to be tested for the presence of prescription drugs amid fears that rivers are being contaminated by the growing quantity of pharmaceuticals flushed unwittingly down the drain.
Powerful anti-cancer drugs are of particular concern as they can be excreted unaltered from the body into the sewerage system.
They are thought to be potentially dangerous because they are highly toxic to dividing cells, are easily dissolved in water and are difficult to destroy by conventional water-treatment techniques.
Scientists are also worried that even if cytotoxic drugs are getting into the water supply at doses too low to affect adults, they may still pose a significant risk to babies in the womb because they would be potentially susceptible to the effects of anti-cancer substances aimed at preventing cell division. "
Britons consume 2,700kg of 5-fluorouracil – just one of 50 cytotoxic drugs. By comparison, they consume about 45kg of the active ingredient of the contraceptive pill, which is believed to be responsible for freshwater fish changing sex.
Scientists in Germany have found pharmaceutical drugs in Berlin's water supply and have called for further research into what could be a Europe-wide problem.
Source: http://www.independent.co.uk/news/science/tests-for-drugs-in-tap-water-945268.html
Recycled Water.
" ...increased
recycling of water in Australia could lead to concerns over the environmental impact of low
concentrations of endocrine disruptors, pharmaceutical drugs and their metabolites, cosmetic
materials, and natural hormones, all have which have been detected in fresh water in Europe
and North America. "
![]() View Latest Live RSS News feed and regular updates relating to Food Poisoning.
View Latest Live RSS News feed and regular updates relating to Food Poisoning.
Latest News and regular updates relating to Food Poisoning.
10th of October 2009
Semi-dried tomatoes linked to hepatitis A
Health authorities recommend semi-dried tomatoes be cooked before being eaten. (ABC News)
A jump in the number of hepatitis A cases in Victoria has been linked to contaminated semi-dried tomatoes.
There have been 12 cases reported in the last week, and the majority have been traced back to the product.
Authorities are working to determine where the contamination came from, and are warning people to
cook semi-dried tomatoes thoroughly before eating them.
Victoria's Chief Health Officer, Dr John Carney, says hepatitis A is a serious illness.
"People present with loss of appetite and general aches and pains, fever chills and then they go
on to get jaundice which is a yellow colouration
of the eyes and skin," he said.
Source: http://www.abc.net.au/news/stories/2009/10/10/2710326.htm
5th of May 2009
Warning on
Semi Dried Tomatoes.
Health Authorities in Victoria and South Australia have advised people not to eat loose semi-dried
tomatoes - in oil with herbs and garlic - that have been purchased from IGA, Foodland, Foodworks
or independent Delis and Cafes.
The warning follows a number of cases of Hepatitis A in both
states that may be associated with the product.
Victoria’s Acting Chief Health Officer, Rosemary Lester, said the move was a precautionary one.
“Although the links between the product and a recent increase in Hepatitis A cases in Victoria are
still under investigation, we have taken this measure in collaboration with our colleagues in SA.
In
the interest of public health, we are therefore advising people not to purchase or consume loose
semi-dried tomatoes in oil with herbs and garlic from these stores. If you have these products at
home, you should throw them out. We are also working with the Victorian manufacturers to
remove this product from these stores across Victoria.”
"Although the links between the product and a recent increase in hepatitis A
cases in Victoria are still under investigation, we have taken this measure in collaboration with our
colleagues in SA," said Victoria's acting Chief Health Officer, Rosemary Lester in a statement.
The suspected tomato product is manufactured in both Victoria and Queensland and sold in
various states by weight. It is sold in supermarkets and is also used by snack bars and cafes
in food preparation.
The Health Departments of South Australia and Victoria have been working closely to identify the
source of the contamination and this work is continuing. The warning does not apply to semi-dried
tomatoes sold in jars, pre-packaged or vacuum packages.
Hepatitis A is spread when traces of faecal matter containing the virus contaminates hands,
objects, water or food and is then taken in by mouth. Symptoms of Hepatitis A include abdominal
pain, nausea, fever and chills and jaundice.
The total number of Hepatitis A cases reported in Victoria this year is 90 compared with 41
reported for the same period last year.
Source: Mnthly Report to the Community Mornington Shire Council May 2009
Source: http://www.abc.net.au/news/stories/2009/05/22/2578480.htm
20th January 2009
EFSA-ECDC report shows Campylobacter cases in humans on the rise, while salmonellosis is in decline; listeriosis remains of concern.
The European Food Safety Authority (EFSA) and the European Centre for Disease Prevention and Control (ECDC)
have published their Community Zoonoses Report for 2007, which analyses the occurrence of infectious diseases
that can be transmitted from animals to humans.
The Report shows that although figures varied considerably
between Member States, Campylobacter infections still topped the list of zoonotic diseases in the
European Union and that the number of cases due to Salmonella infections in humans fell for the fourth year
in a row. Cases of listeriosis remained at the same level.
In foodstuffs, Campylobacter, which generally causes diarrhoea, cramps and fever in humans, was mostly
found in raw poultry meat with an average of 26% of samples showing contamination.
In live animals,
Campylobacter was found in poultry, pigs and cattle.
Poultry and pig meat were reported as the foods most frequently associated with Salmonella, and on
average 5.5 % of all fresh poultry meat samples within the European Union was found to be contaminated.
Eggs and egg products were also found to be contaminated, while the bacterium was only rarely detected in
raw dairy products, vegetables and fruits. In animal populations, Salmonella was most frequently detected
in poultry flocks.
Source: Press Releases & News Stories European Food Safety Authority http://www.efsa.europa.eu/
01 October 2008
Update: Deadly listeriosis outbreak.
The number of confirmed deaths linked to the listeriosis outbreak traced to a Maple Leaf Foods meat-packing plant in Toronto has risen to 20.
Six deaths across the country are still under investigation.
In August, Maple Leaf Foods issued a recall of virtually all the products produced at the Toronto plant after the deadly listeriosis outbreak was made public.
03 Sep 2008
Pre-packed salad 'will lead to increased food poisoning'
Scientists warned that the increasing popularity of pre-packed salad sold by supermarkets, could lead to a rise in food poisoning.
Researchers have discovered how salmonella and E.coli germs - more commonly associated with chicken and bovine products - can spread to salad and vegetable leaves.
Professor Gadi Frankel carried out research, with the University of Birmingham and found that salmonella bacteria are able to use their flagella - the stringy “propellors” designed to aid their movement - to grip salad leaves and contaminate them.
Professor Gadi Frankel, from Imperial College, said consumers needed to be aware of the risk of contaminated salad to avoid potential food poisoning.
"In their efforts to eat healthily, people are eating more salad products, choosing to buy organic brands and preferring the ease of 'pre-washed' bagged salads from supermarkets, than ever before," he said.
Salmonella and E.coli live in the gut of cows and egg-ducts of chickens, and contamination of meat can occur during slaughtering but recent outbreaks of food poisoning highlight the dangers associated with contaminated salad or vegetables.
Scientists know that salmonella and E.coli 0157 - a strain that can cause serious sickness in humans - can spread to salads and vegetables if they are fertilised with contaminated manure or come into contact with contaminated products.
Just because some labels claimed food was pre-washed did not necessarily make it safe to eat.
"All of these factors, together with the globalisation of the food market, mean that cases of salmonella and E.coli poisoning caused by salads are likely to rise in the future."
A salmonella outbreak in the UK in 2007 was traced back to imported basil while an E.coli outbreak in America in 2006 was linked back to pre-packed baby spinach.
http://www3.imperial.ac.uk/newsandeventspggrp/imperialcollege/newssummary/news_3-9-2008-10-4-59
01/02/2003 Salmonella Melbourne Australia
A mayonnaise spread made at a Vietnamese and Chinese Restaurant was found to contain salmonella strains
that have to one death and 106 people becoming infected with gastroenteritis.
The spread was made from
oil, raw eggs and garlic flakes, and was used on the restaurant’s pork rolls and chicken rolls.
The dead Doncaster man died in his home 3 days after eating the pork roll.
His mother was also infected
and was admitted to hospital with food poisoning symptoms.
Nearly all people infected had eaten a pork
or chicken roll from the restaurant. The youngest victim of the outbreak was only 2 years old, and the
oldest was an 80 year old woman.
Victoria's Deputy Chief Health Officer said that the rolls were sold
at room temperature, and high temperatures in Melbourne were likely to have helped the bacteria
multiply. One infected victim claimed that "one utensil was being used to pick up all sorts of
ingredients."
Victims suffered from diarrhoea, vomiting and stomach cramps.
25/03/2002 Bacillus cereus. Melbourne Australia
Contaminated rice is believed to be the cause of severe food poisoning that hit more than 250 people
celebrating the Islamic New Year in Melbourne's northern suburbs.
Health authorities tested samples of
the suspect rice and other food served at the festival after 10 hospitals and medical centres were
flooded with violently ill people.
The outbreak was the worst mass food poisoning in Victoria since
1997 when more than 550 people fell ill after eating pork rolls infected with salmonella.
Initial tests on rice dishes indicated the likely bacterial germ was bacillus cereus.
01/04/1999 Salmonella Typhimurium 135a. Adelaide Australia
An outbreak of Salmonella Typhimurium 135a strain contamination in Adelaide caused 486 reported cases
of food poisining.
The South Australian Health Commission said tests from a Riverland citrus packing
shed had come up positive to the same salmonella strain found in the product of an Adelaide orange
juice company.
At the same time in Victoria, a salmonella outbreak caused the death of a man, 74, and twenty-one
cases of illness. The interstate outbreak was not officially proven linked to SA at the time.
01/07/1998 Cryptosporidium and Giardia parasites. Sydney Australia
A three-month water supply contamination crisis affected Sydney and region following cases of illness
caused by Cryptosporidium and Giardia parasites in some Sydney reservoirs. The NSW Health Department,
however, reported that there was no signficant increase in illness reported.
A major cost to Sydney Water Corporation was almost $20m in $15 rebates on consumers' next water bill
which were given for the inconvenience of not being able to drink tap water before boiling it.
Sydney Water also paid out some $14m in insurance claims and $12.5m for monitoring and testing.
The five volume report on the incident cost $2m.
Legal class action was taken by businesses for loss of business and one law firm reported they
had 'heard' from just over 100 individuals who believed they became sick as a result of the water contamination.
The final total estimated cost reported by Sydney Water Corporation was $75 m.
People Affected 4,000,000
01/11/1994 to 01/02/1995 Adelaide Australia
One child died and many were hospitalised after eating "Garibaldi" brand smallgoods over the
Christmas 1994 holiday period.
The common denominator was found to be Garibaldi's metwurst product,
a fermented meat product which is not cooked but just fermented and seasoned.
The dead child was a
4 year old girl, and 22 people were hospitalised. most of those who were hospitalised were children,
whose immature system could not cope with the efects of the food poisoning.
The illnes caused kidney
and other systemic failures, resulting in long hospitalisations and life-long ongoing illness.
Source: EMERGENCY MANAGEMENT AUSTRALIA,
[Return to Top]
Australia fourth in world food safety rankings 2008
Australia is in the top five Organisation for Economic cooperation and Development nations with the safest food supplies, according to a study conducted by Canadian academics.
The ‘Food Safety Performance World Ranking 2008’ placed the UK first and Australia fourth, one ahead of Canada, but all the top five ranked as having ‘superior’ performance.
Of 17 countries in the study, those listed from sixth to fourteenth were ‘average’ while the last three were rated ‘poor’.
The United States was seventh.
The full list:
1. United Kingdom (5) Superior
2. Japan (2) Superior
3. Denmark (28) Superior
4. Australia (14) Superior
5. Canada (9) Superior
6. Finland (33) Average
7. United States (1) Average
8. Switzerland (20) Average
9. Norway (25) Average
10. Germany (3) Average
11. Italy (7) Average
12. Netherlands (16) Average
13. Sweden (19) Average
14. Austria (26) Average
15. France (6) Poor
16. Belgium (18) Poor
17. Ireland (31) Poor
The numbers in brackets show the country’s world ranking based on GDP (Nominal) in 2007.
newsroom/foodstandardsnews/foodstandardsnews65w3965.cfm#_australia
[Return to Top]
Deliberate Additon of unsafe products to our food
Deliberate Food adulteration is an act of adding or mixing something inferior, harmful, useless and unnecessary to food.
It is intended to reduce manufacturing cost, increase bulk or weight, make it appear better and conceal inferiority.
Historical Introduction.
Some of the commonly used additives in the 19th century were poisonous. To
whiten bread, for example, bakers sometimes added alum
and chalk to the flour, while mashed potatoes, plaster of Paris (calcium
sulphate), pipe clay and even sawdust could be added to increase the weight of
their loaves.
Rye flour or dried powdered beans could be used to replace wheat
flour and the sour taste of stale flour could be disguised with ammonium
carbonate. Brewers too, often added mixtures of bitter substances, some
containing poisons like strychnine, to ‘improve’ the taste of the beer and save
on the cost of hops.
Of all forms of adulteration the most reprehensible was the use of poisonous
colouring matters in the manufacture of jellies and sweets. The bright colours
used to attract children often contained lead, copper or mercury salts. "
" But of all possible nefarious traffic and deception, practised by mercenary dealers, that of adulterating the articles intended for human food with
ingredients deleterious to health, is the most criminal, and, in the mind of every honest man, must excite feelings of regret and disgust. "
F. Accum, A treatise on adulterations of food and culinary poisons. London: Longman, 1820.
Food Poisoning and Food Adulteration in the 21st century.
Adulteration and globalisation
" According to the European Food Safety Authority, the world is facing a number
of significant changes which will impact on food safety.
Not least, the globalisation of world markets will increase the
likelihood of new or re-emerging risks, while climate change and the
sustainability of food production practices will necessitate a more integrated
approach to risk assessment that addresses risks along the entire food chain.
The adulteration of milk with melamine in China is an example of the problems
food marketers will have to deal with.
Melamine is used in the plastics industry and should not be used in food.
While Chinese authorities are still
investigating the circumstances surrounding the melamine-contaminated milk, it
is thought that melamine was added at milk collection depots to mask the fact
that it had been watered down.
As the food industry becomes increasingly globalised the potential for crises
similar to the Chinese milk adulteration, in both raw and processed foods,
increases.
Ethical companies are going to have to be even more vigilant to
ensure the identity and quality raw and processed foods they import.
The
melamine in milk scandal provides a salient warning that companies cannot
simply rely on unsophisticated laboratory results to confirm the quality of an
ingredient.
They will need to develop testing and scrutiny procedures to
overcome the potential for deliberate adulteration in the global marketplace. "
Deliberate Food Adulteration at a Hotel in Syney, Australia
" The New South Wales Government says an ice-cream sample at the centre of a contamination row has tested positive for faecal matter.
Two families say staff served them ice-cream laced with human excrement at the Coogee Bay Hotel, in eastern Sydney, on October 5th.(2008)
They say they received the dessert free of charge after complaining they could not hear the televised rugby league grand final over the pub's music.
Stephen and Jessica Whyte reportedly went to the police after tasting the ice-cream and then had the food tested at an independent laboratory, which confirmed it was contaminated with faecal matter."
Source: http://www.abc.net.au/news/stories/2008/10/29/2404427.htm
Food Adulteration On the Rise in Ghana 1 September 2008
" Mrs. Isabella Mansa Agra, Head of Food Registration and Nutrition of the FDB,
in a document copied to the Ghana News Agency,
said food adulteration was on the increase and common in Ghanaian urban markets with the perpetrators playing
on the ignorance of innocent buyers.
She said the survey revealed that alum and chalk were added to bread to whiten
it, while for stale flour, ammonium carbonate was added to disguise its sour
taste. Mashed potatoes, sawdust and Plaster of Paris were also added to
increase the weight of the bread.
Mrs Agra noted that food dyes, colours and miscellaneous compounds were added
to food to impart certain properties to disguise deteriorated or spoiled food
and give an idea of freshness. "
Source: http://allafrica.com/
Adulteration of Food. A Deep Rooted Social Evil
January 25, 2001
" We toil day and night for what? For that two morsel of wholesome nutritive food.
And if at the end of the day we are not sure of what we eat, than what are we toiling for?
We may be eating a dangerous dye, sawdust, soap stone,
industrial starch, Aluminum foil and believe it, even horse-dung! Inviting
disease rather than good health.
And what are the law enforcing authorities
doing? Looking the other way, ignoring, sitting on files and being bought and
bribed. "
Source: http://news.boloji.com/index.htm
Meat Safety - Glowing Meat.
Meat surfaces glow in the dark or in refrigerators.
The glow may vary from white and clear to bluish green.
The glow may resemble studded stars on meat surfaces or the glow may appear on chiller walls.
Certain bacteria have the power to produce light and are known as photobacteria.
A common type is Pseudomonas phosphorescens and is widely distributed in nature.
The presence of phosphorescence on meat is not in itself injurious to the consumer although it may be an indication of unsanitary conditions requiring attention such as cleaning a refrigerator or carrying out clean handling techniques.
The storing of fish in the same chiller may contribute to phosphorescence development.
The meat surface can be trimmed.
However as the bacteria causing the glow will fade as the meat deteriorates, the meat may need to be assessed to determine if it is safe and suitable to eat.
Source: http://www.health.wa.gov.au/envirohealth/food/glowingmeat.cfm