Flesh-eating ulcer bacteria in Australia.

before devouring muscle tissue to the bone.(1)
Flesh-eating ulcer, Mycobacterium ulcerans on the increase.
 " An outbreak of a flesh-eating bacteria that can lead to limb amputations is plaguing several Victorian coastal towns.
The Bairnsdale ulcer outbreak is shaping to be the worst on record and there are fears the bacteria could be spreading."
Barwon Health deputy director of infectious diseases Daniel O'Brien said the condition had been detected from East Gippsland to Frankston and there was a also a strong concentration on the Bellarine Peninsula.(2) "
" An outbreak of a flesh-eating bacteria that can lead to limb amputations is plaguing several Victorian coastal towns.
The Bairnsdale ulcer outbreak is shaping to be the worst on record and there are fears the bacteria could be spreading."
Barwon Health deputy director of infectious diseases Daniel O'Brien said the condition had been detected from East Gippsland to Frankston and there was a also a strong concentration on the Bellarine Peninsula.(2) "
 Select an article on this page.
Select an article on this page.
1: Introduction:
2: Mycobacterium ulcerans in Victoria.
3: Mycobacterium ulcerans in New South Wales.
4: Daintree ulcer in Queensland.
5: Causes and spread of the disease to humans.
6: Symptoms of the disease.
7: Mycobacterium ulcerans in dogs and wildlife.
Introduction.
Buruli ulcer ( also named Bairnsdale ulcer and Daintree ulcer according to their respective Australian region ) is an emerging human disease caused by infection with
a slow-growing pathogen, Mycobacterium ulcerans, that produces mycolactone,
a cytotoxin with immunomodulatory properties.(3)
It is the third most common mycobacterial disease after tuberculosis and leprosy.(4)
In the popular press the infection is sometimes called the “the flesh-eating bug”.The Mycobaterium Ulcerans first appears as an ulcer or a pimple, which produces a toxin
that eats away at the skin and muscles, destroying the soft tissue.
This toxin overwhelms the immune system response, allowing it to spread to all over the body and down to the bone.
In 1897, Sir Albert Cook, a British physician working at the Mengo Hospital in Kampala,
Uganda, described skin ulcers that were consistent with Buruli ulcer (BU).(5)
In 1948, Professor Peter MacCallum and his colleagues in Australia provided a detailed
description of the disease among six patients from the Bairnsdale area near Melbourne.
They were the first scientists to isolate the causative organism, Mycobacterium ulcerans.
In southern Australia, the disease is still referred to as the Bairnsdale ulcer.
In Australia it was first diagnosed in the Bairnsdale area of East Gippsland where
an outbreak of 120 cases occurred in the 1940’s and became known as "Bairnsdale Ulcer".(6)
It has also been found in far north Queensland (Daintree region) and near Rockhampton and Darwin. (7)
but is most common in West Africa where thousands of cases have been recorded. All countries along the Gulf of Guinea are affected.
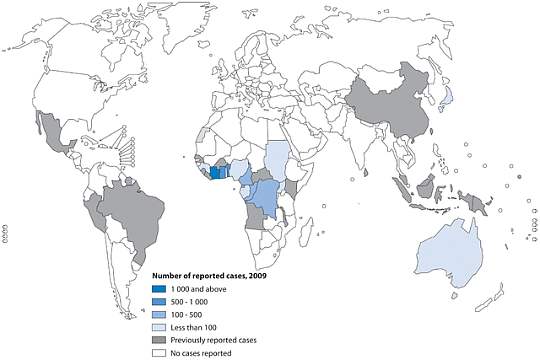
Small numbers of cases have also been
reported from Japan, China and Malaysia, indicating that the disease may be more widespread in the
Western Pacific region than is currently recognised. In 2005, the first case of BU aquired in the
state of New South Wales (NSW) was diagnosed. In Victoria, cases of BU have also been described in
several marsupial species, including koalas, potoroos and possums and in 2006, the first cases in
horses and a cat were documented.(9)
Mycobacterium ulcerans in Victoria.
The spread of Mycobacterium ulcerans westwards.
Until 1982 to 1983, when three cases were detected near Western Port Bay, cases in Victoria
were confined to the Bairnsdale area. Since 1983, over 50 cases have been recorded in Victoria
outside this area, and the disease appears to be spreading progressively westward.
An outbreak on Phillip Island in 1993 and 1994 resulted in 27 reported cases.
From 1990 to 1997, 22 cases within approximately 70 km of Melbourne were reported, 19 of these
on the Mornington Peninsula with 12 in the Frankston/Langwarrin area (Figure).
For the first time,
cases were detected west of Melbourne in 1998, and the number occurring in that area is
increasing.
Source:Mycobacterium ulcerans Treatment Costs,
Australia Accessed 29/12/2011
http://wwwnc.cdc.gov/eid/article/10/6/03-0428_article.htm
South-east Australia is the only non-tropical area in the world where the
Bairnsdale ulcer is detected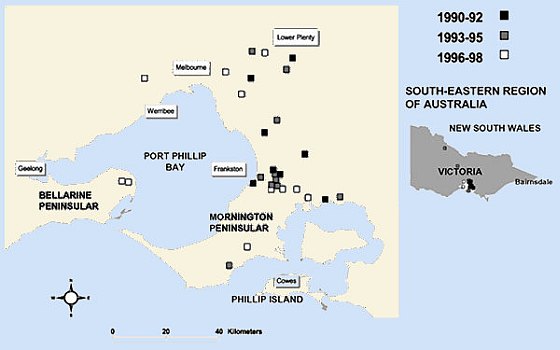
There has been an increase
of reported human Mycobacterium ulcerans infections within
the Bellarine Peninsular region.January 1998–May 2017

Locations (circles) of 426 cases of Mycobacterium ulcerans disease in Bellarine and Mornington Peninsulas, Barwon Health Cohort, Geelong, Victoria, Australia, January 1998–May 2017. Size of circles indicates number of cases, given in parentheses. Box in inset shows study region in southeastern Australia.
Emerg Infect Dis. 2018;24(1):58-64 (16)
| Location | Total cases | Mean no. cases per year | Resident population | Mean annual incidence (95% CI) |
| Barwon Heads | 13 | 2.6 | 2,993 | 0.87 (0–1.95) |
| Breamlea | 0 | 0 | 244 | 0 (0–0.012) |
| Geelong | 5 | 1 | 160,991 | 0.01 (0–0.74) |
| Ocean Grove | 10 | 2 | 11,274 | 0.18 (0–1.44) |
| Point Lonsdale | 50 | 10 | 2,477 | 4.04 (0.81–6.4) |
| St Leonards | 3 | 0.6 | 1,621 | 0.37 (0–0.43) |
| Wallington | 0 | 0 | 1,353 | 0 (0–0.003) |
http://wwwnc.cdc.gov/eid/article/10/6/03-0428_article.htm
Media Release. April 16, 2018
Victoria battles flesh-eating bug epidemic.
Victoria battles flesh-eating bug epidemic
A flesh-eating bug is on the rise in regional Victoria and researchers don't know how it's spreading.
Victoria is facing a worsening epidemic, with 182 new cases in 2016, 275 in 2017 and 30 so far in 2018.
The cases are also becoming more severe and occurring in new areas, but efforts to control the outbreak have been thwarted, because it's not known how humans are infected, a study published in the The Medical Journal of Australia on Monday says.
Native and domestic animals, including dogs, cats, possums and koalas, have all developed the disease, but it's unknown whether they spread it.
"As a community, we are facing a rapidly worsening epidemic of a severe disease without knowing how to prevent it," researchers said.(17)
Media Release. December 08, 2011
The Barwon Health deputy director of infectious diseases Associate Professor O'Brien said there have
been 42 cases of Bairnsdale ulcer in the Barwon South Western region in the past 12 months.
The figure represents well over half the total number of cases in the state for the same period.
Eleven of the local cases are from the tiny Borough of Queenscliff, at the tip of the Bellarine Peninsula.
The organism responsible for Bairnsdale ulcer has been found in patches of swampy soil o
n the Bellarine Peninsula.
Point Lonsdale, Queenscliff, Barwon Heads and Ocean Grove are hot-spots.
While the disease was uncommon in the rest of the country, it was at epidemic levels in the Geelong region, he said.
Source:Geelong Advertiser Accessed 29/12/2011
http://www.geelongadvertiser.com.au/article/2011/12/08/296241_news.html
Media Release. November 25th, 2011
BARWON Health authorities have been flat out dealing with their worst outbreak ever of Bairnsdale ulcer.
Over 40 cases of the flesh-eating bug have been diagnosed in the Barwon South Western region this year, up from 15 in the same period in 2010.
The head of Barwon Health's department of infectious diseases, Professor Eugene Athan, said the Bellarine Peninsula was again the state hotspot for Bairnsdale ulcer.
He said it was important to diagnose the problem early, and those that went undiagnosed were harder to cure and often left scars.
Source:Geelong Advertiser Accessed 29/12/2011
http://www.geelongadvertiser.com.au/article/2011/11/25/293701_news.htm
Media Release. August 31, 2011
"I don't want people to panic and suddenly avoid the Bellarine Peninsula as a holiday place,
it's just about trying to raise awareness of the organism," Associate Professor O'Brien said.
Associate Professor O'Brien said the worst cases seen in Australia could result in skin grafts, while amputations occurred in Africa when the infection was left to fester.
The bacteria, when detected early, can usually be treated with a unique antibiotic and wound dressings.
The Barwon Health deputy director of infectious diseases Associate Professor O'Brien said 35 cases
had been recorded in Victoria this year compared with 20 at the same time last year and urged residents
of affected areas, as well as visitors, to remain vigilant.
The bacteria is thought to be spread mostly by mosquitoes, but could also be caused by sandflies and
other insects, or through cuts caused by thorns or bushes. Cuts that come in contact with mud or dirt
can also become infected.
"We've had a pretty wet autumn and winter so the concern is that we may see more cases and that
people at the moment may be getting exposed and infected because of a high number of mosquitoes.
"I don't think we've ever seen as many cases anywhere in Australia as we see now in the Bellarine Peninsula." Twenty-five of the reported cases in Victoria this year have occurred in the Bellarine Peninsula,
only five less than the record number of cases for the region recorded in 2005.
Twenty-five of the reported cases in Victoria this year have occurred in the Bellarine Peninsula,
only five less than the record number of cases for the region recorded in 2005.
During the past two years, the number of infections affecting children under five has more than doubled
to about 10 per cent of all Bellarine Peninsula cases.
There can be a three to six-month gap between the time of infection and symptoms occurring,
so most people are likely to have become infected during the steamy end to summer. [Return to Top]
Associate Professor O'Brien said it was important that people who travelled through these areas were aware the bacteria existed.
"If you look at history, it's sort of gradually been spreading west," he said.
"These places are coastal, they're similar environments and we need to remain vigilant and keep an eye out for cases developing in these areas.
"The problem is outside of these areas it doesn't really occur so most medical doctors and nurses would have never seen one."
South-east Australia is the only non-tropical area in the world where the Bairnsdale ulcer is detected. Areas of Queensland and the Northern Territory have recorded cases.
Source:The Age August 31, 2011 Accessed 29/12/2011
http://www.theage.com.au/victoria/flesheating-ulcer-cases-jump-20110831-1jl7m.html
Media Release. August 26, 2011
A Geelong doctor is warning about a sharp rise in the number of cases of a flesh-eating ulcer on the Bellarine Peninsula.
The number of people contracting Bairnsdale ulcers has jumped from an average of one a month, to 15.
If the ulcer is left untreated, it can eat away skin and destroy bones.
The cause is not known but it is thought to be contracted from skin cuts or mosquito bites
Source:Australian Broadcasting Corporation August 26, 2011 Accessed 28/12/2011
http://www.abc.net.au/news/2011-08-26/warning-over-sharp-rise-in-bairsndale-ulcer-cases/2856790
Mycobacterium ulcerans in New South Wales
First case of Mycobacterium ulcerans disease (Bairnsdale or Buruli ulcer) acquired
in New South Wales.
M. ulcerans is an environmental pathogen, which is transmitted by an unknown
mechanismn to humans who enter endemic areas.
It is not surprising that M. ulcerans exists in coastal environments in southern NSW, just as it does in Victoria. There have also been cases of Buruli ulcer from Mallacoota (unpublished data), a small town in eastern Victoria adjacent to the NSW border The rarity of cases in NSW compared with Victoria remains unexplained.
It is unlikely to result from failure to recognise
previous cases in NSW, as the progressive nature of the infection means that most
cases are eventually diagnosed. Australian primary care clinicians need to be
aware that Buruli ulcer may occur in NSW, to ensure early diagnosis and treatment
to minimise disability.

(20) Source: Medical Journal of Australia
Media Release. January 14, 2007
The flesh-eating Daintree Ulcer has struck again, this time in NSW where a sea kayaker developed a gaping wound on his ankle.
The 42-year-old man's ankle became infected while sea kayaking off the town of Eden in southern NSW.
A scab on his ankle developed into a large, open wound that continued to grow over five months before the ulcer was excised by Melbourne surgeons early last year.
Source:The Courier-Mail January 14, 2007 Accessed 28/12/2011
Mycobacterium ulcerans in Queensland.
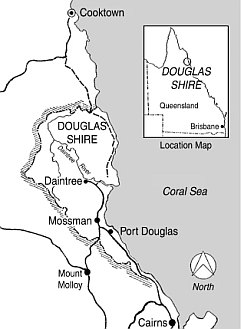 The
Daintree River catchment in north Queensland is an endemic focus for Mycobacterium ulcerans ‘Daintree ulcer’ infection and has been a long-standing health problem for
the people of this well-circumscribed region of North Queensland
from prior to European settlement. The indigenous people of the Mossman–Daintree area have been
aware of this disease entity long before European settlement, and
there are numerous anecdotal reports.(10)
The
Daintree River catchment in north Queensland is an endemic focus for Mycobacterium ulcerans ‘Daintree ulcer’ infection and has been a long-standing health problem for
the people of this well-circumscribed region of North Queensland
from prior to European settlement. The indigenous people of the Mossman–Daintree area have been
aware of this disease entity long before European settlement, and
there are numerous anecdotal reports.(10)
In 1942, Cilento described possible M. ulcerans infections from around
Rockhampton. Four other culture-confirmed cases were reported between 1957 and
1962 from the Glass House Mountains (Sunshine Coast) and Maryborough (Fraser
Coast) regions in Queensland. Four cases occurred within a small geographic
area centred on Yeppoon and the suburbs of Rockhampton ( North Rockhampton Sep
2000, Yeppoon Jun 2003, Bungundarra Aug 2004, Keppel Sands Nov 2004.)(11)
From 1964 to 1990, there were 27 cases and from 1991 to 2008, there
were 65 cases. It is still an uncommon infection in this region, with one to four
cases per year most years.(10) although the increase in cases in Victoria raises the possibility of a potentially similar dramatic increase in cases in central Queensland.
Media Release. May 17, 2000
An area around Mossman just north of Cairns is Australia's hot-spot for the disease, with about 70 cases diagnosed since the early 1960s.
Mossman Hospital Director of Nursing, May Smith and the Cairns Base Hospital Director of Surgery, Doctor Christina Steffen, are next month travelling to the World Health Organisation's Geneva headquarters for a workshop about the bacteria.
Scientists don't know how people catch myco-bacterium ulcerans, they don't know where it resides in the environment and they don't know how it can spread. But Doctor Christina Steffen says it's not the only fleshing eating bacteria in the world.
But in the past 50 years about 70 cases have been diagnosed around Mossman and the rate is rising, with most of the cases in the last decade.
May Smith said "...in 1952 when I was a student nurse here at Mossman Hospital, we had a little four year old Aboriginal girl who had an ulcer on her elbow that was eaten right into the bone, and at that time we thought it was what's called yores [phonetic], that's a disease that's found in Papua New Guinea. And I'd have to dress this wound, and we used to have to debride it and clean it up every day. And I would be scratching away at that wound and the little girl would be just looking at me and not even wincing with pain, and I knew - and so we all knew that there was something really strange about it. Well, she spent about four years in hospital."
Source: Australian Broadcasting Corporation
http://www.abc.net.au/pm/stories/s127969.htm Accessed 28/12/2011
Causes and spread of the disease to humans.
How people become infected with Mycobacterium ulcerans is not completely understood,
but numerous studies have explored the role of biting insects.
" In 2007, it was discovered that M. ulcerans could be detected in association with mosquitoes trapped in one town in southeastern Australia during a large outbreak of BU.
Adult mosquitoes were trapped in seven towns on the Bellarine Peninsula in Victoria, Australia,
from December 2004 to December 2009 and screened for M. ulcerans by real-time PCR.(12)
The number of laboratory-confirmed cases of BU in permanent residents of these towns diagnosed
during the same period was tallied to determine the average cumulative incidence of BU in each location.
Pearson's correlation coefficient (r) was calculated for the proportion of M. ulcerans-positive
mosquitoes per town correlated with the incidence of BU per town.
We found a strong dose-response relationship between the detection of M. ulcerans in mosquitoes
and the risk of human disease.
We found a strong association between
the proportion of M. ulcerans-positive mosquitoes and the incidence of human disease.
The results of this study strengthen the hypothesis that mosquitoes are involved in the transmission
of M. ulcerans in southeastern Australia. This has implications for the development of strategies to control and prevent Mycobacterium ulcerans."
Source:Published online 2011 September 20. doi: 10.1371/journal.pntd.0001305 http://dx.crossref.org/10.1371%2Fjournal.pntd.0001305 Accessed 29/12/2011
Associate Professor O'Brien deputy director of infectious diseases at Barwon Health said the bacteria, is thought to be spread mostly by mosquitoes, but could also be caused by sandflies and other insects, or through cuts caused by thorns or bushes. Cuts that come in contact with mud or dirt can also become infected.
Source:The Age August 31, 2011 Accessed 29/12/2011
http://www.theage.com.au/victoria/flesheating-ulcer-cases-jump-20110831-1jl7m.html
Symptoms of the disease.
Symptoms of the Mycobacterium ulcerans ‘Bairnsdale ulcer’.
The progression of symptoms can include:
• A spot that looks like a mosquito bite forms on the skin.
• The spot grows bigger over days or weeks.
• The spot may form a crusty, non-healing scab.
• The scab then disintegrates into an ulcer.
• The ulcer continues to enlarge.
Unlike other ulcers, this ulcer is usually painless and there is generally no fever or other signs of infection.
The limbs are more commonly affected.
The infection may sometimes present as localised pain and swelling with fever but no ulceration.
 At the first stage of an Mycobacterium ulcerans infection a spot that looks like a mosquito bite forms on the skin.
At the first stage of an Mycobacterium ulcerans infection a spot that looks like a mosquito bite forms on the skin.
 The toxins made by the bacteria ( mycolactone, a cytotoxin with immunomodulatory properties ) destroy skin cells, small blood vessels and subcutaneous fat, which causes ulceration and skin loss. In severe cases, the infection can destroy bone.
The toxins made by the bacteria ( mycolactone, a cytotoxin with immunomodulatory properties ) destroy skin cells, small blood vessels and subcutaneous fat, which causes ulceration and skin loss. In severe cases, the infection can destroy bone.
Since the ulcer gets bigger with time, early diagnosis and prompt treatment can keep the amount of skin loss to a minimum.
Source: Bairnsdale ulcer Fact Sheet Better Health Channel
http://www.betterhealth.vic.gov.au Accessed 29/12/2011
Mycobacterium ulcerans in dogs and wildlife.
In Victoria, cases of BU have also been described in native wildlife and domestic mammal species, including koalas (Phascolarctos cinereus), common ringtail possums (Pseudocheirus peregrinus), a mountain brushtail possum (Trichosurus cunninghami), a long-footed potoroo (Potorous longipes), two horses(13), five dogs(14), an alpaca and a cat(15). All animal cases were identified in locations where human cases of BU have been reported.
Dr Janet Fyfe,of the Victorian Infectious Diseases Reference Laboratory, Australia
has investigated the possible environmental sources of M. ulcerans in Point
Lonsdale, where over one-hundred human BU cases have been diagnosed since 2002.
The highest concentrations M. ulcerans DNA detected were found in the faeces of
ringtail and brushtail possums.
After examining and sampling of live captured possums in Point Lonsdale
it was revealed that 38% of ringtail possums and 24% of brushtail possums,
respectively, had laboratory-confirmed M. ulcerans lesions and/or M. ulcerans
PCR-positive faeces.
Several of the infected ringtail possums had multiple skin lesions and signs of
systemic infection. This finding raises the possibility that mammals may be an
environmental reservoir for M. ulcerans.
The way in which M. ulcerans might be transmitted from an animal to humans is not
clear, and likely to be indirect.
Dr Janet Fyfe, proposes that the transmission pathway may involve vegetation,
vertebrate hosts and invertebrate vectors eg. biting insects. Such a model
represents a fundamental change to the existing views on the ecology of M.
ulcerans.
Source:Bairnsdale/Buruli Ulcer: From Possums To People
Dr Janet Fyfe, Victorian Infectious Diseases Reference Laboratory, Australia
The Australian Society for Microbiology, Annual Scientific Meeting (ASM2011)
4–8 July 2011 Accessed 29/12/2011
http://www.asm2011.org/
Media Release. January 09, 2009
Dog diagnosed with flesh-eating Bairnsdale ulcer.
Bellarine residents and pet owners have been warned to keep a close eye on suspicious bites that refuse to heal after a Point Lonsdale dog was diagnosed with the aggressive Bairnsdale ulcer.
The diagnosis in "Jack" the kelpie is the first confirmed finding of the flesh-eating bug in dogs, proving it can affect horses, cats, possums and alpacas as well as humans.
Mosquitoes were thought to be a factor in the spread of the bug but Barwon Health infectious disease specialist Dr Daniel O'Brien said he was not convinced the biting insects were the sole carriers of the infection.
"We know it's in the soil and it comes up more commonly when it's wet and there's a lot of water," Dr O'Brien said.
"People that have exposed areas, wearing shorts and T-shirts, may be getting bitten by mosquitoes and getting the disease, but others are maybe getting soil on them and the bug on them or into open wounds.
"The only way we can advise people to prevent infection is to avoid mosquito bites and cover up when working with soil."
The Bairnsdale ulcer, also known as the flesh-eating bug, is found in many parts of the world, however it is only in coastal Victoria where the infection appears in animals.
Dr McMillan of the Bellarine Animal Hospital said DNA testing proved it was the same condition that infected humans and that he had consulted Barwon Health specialists to find out treatments for Bairnsdale ulcer.
He said testing of several environmental factors near the dog's home had proved the bug was present in the area but it was not know how Jack came to be infected.
"The owner noticed what looked like a small mosquito bite on the dog and over time it didn't heal and was getting worse and starting to ulcerate," Dr McMillan said.
"We made sure it wasn't a grass seed, which is the most common cause of these sorts of problems. When that was ruled out we did some swabs and a lab confirmed it."
Source:Geelong Advertiser Accessed 29/12/2011
http://www.geelongadvertiser.com.au/article/2009/01/09/42825_news.html

Other Articles:
1: Australian Venomous Ants.
2: Most venomous snake in the world: Found only in Australia.
3: Is there a risk of a volcanic eruption in Australia ?
4: Summary of Major Bush Fires in Australia Since 1851.
5: Chronology of Australian Major Droughts.
6: Early Settlers' Homes and Bush Huts in Australia.
References and other Sources:
Reference and Sources:
(1) Source: Map constructed from available data.
(2) Source: Geelong Advertiser
http://www.geelongadvertiser.com.au/article/2011/12/08/296241_news.html Accessed 29/12/2011
(3) Source: Nature Reviews Microbiology 7, 50-60 (January 2009) | doi:10.1038/nrmicro2077
Buruli ulcer: Reductive evolution enhances pathogenicity of Mycobacterium ulcerans -
Caroline Demangel, Timothy P. Stinear & Stewart T. Cole Accessed 28/12/2011
(4) Source: Qi W, Käser M, Röltgen K, Yeboah-Manu D, Pluschke G (2009) Genomic Diversity and Evolution of Mycobacterium ulcerans Revealed by Next-Generation Sequencing. PLoS Pathog 5(9): e1000580. doi:10.1371/journal.ppat.1000580
Editor: Edward C. Holmes, The Pennsylvania State University, United States of America
Published: September 11, 2009 Accessed 25/12/2011
(5) Source: Mycobacterium ulcerans infection Fact sheet N°199 Revised March 2007
World Health Organization http://www.who.int/entity/mediacentre/factsheets/en/ Buruli ulcer disease Accessed 28/12/2011
(6) Source: Bairnsdale ulcer. Department of Health Victoria
Diseases http://ideas.health.vic.gov.au/diseases.asp Accessed 25/12/2011
(7) Source:
http://ideas.health.vic.gov.au/diseases/mycobacterium-ulcerans-facts.asp and (10)
Accessed 28/12/2011
(8) Source: Map sourced from World Health Organization
(9) Source: see ( 15 )
(10) Source: Mycobacterium ulcerans infection in North Queensland:
the ‘Daintree ulcer’ Accessed 28/12/2011
Christina M. Steffen,* May Smith† and William J. H. McBride*
*James Cook University, School of Medicine and Dentistry, Clinical School, Cairns Base Hospital, Cairns, Queensland, Australia
†Queensland Health, Mossman Hospital, Mossman, Queensland, Australia/ Accessed 30/12/2011
(11) Source: Francis G, Whitby M, Woods M. Mycobacterium ulcerans infection: a
rediscovered focus in the Capricorn Coast region of central Queensland
[letter]. Med J Aust 2006; 185: 179-180. Accessed 28/12/2011
(12) Source: Risk of Buruli Ulcer and Detection of Mycobacterium ulcerans in Mosquitoes in Southeastern Australia.
Caroline J. Lavender, Janet A. M. Fyfe, Joseph Azuolas, Karen Brown, Rachel N. Evans, Lyndon R. Ray, and Paul D. R. Johnson Published online 2011 September 20. doi: 10.1371/journal.pntd.0001305 Accessed 28/12/2011
(13) van Zyl, A., et al., Mycobacterium ulcerans infections in two horses in south-eastern
Australia. Aust Vet J, 2010. 88(3): p. 101-106.
(14) O'Brien, C.R., et al., Localised Mycobacterium ulcerans infection in four dogs. Aust Vet J
(in press).
(15) Elsner, L., et al., Localised Mycobacterium ulcerans infection in a cat in Australia. J Feline
Med Surg, 2008.
(16) Source: First Case of Mycobacterium ulcerans Disease (Buruli Ulcer) Following a Human Bite Accessed 28/12/2011
http://cid.oxfordjournals.org/content/36/5/e67.full
Further Reading:
• Drummond C, Butler, JRG. Mycobacterium
ulcerans treatment costs, self-reported data, Australia. Emerging Infectious Diseases. 2004 Jun. Available from: http://wwwnc.cdc.gov/eid/article/10/6/03-0428.htm
• Francis G, Whitby M, Woods M. Mycobacterium ulcerans infection: a rediscovered focus in the Capricorn Coast region of central Queensland. Med J Aust. 2006;185:179–180. [PubMed]
• Infectious diseases,
epidemiology and surveillance.
http://docs.health.vic.gov.au/docs/doc/Surveillance-of-notifiable-infectious-diseases-in-Victoria-2006-Mycobacterial-infections
• Jenkin GA, Smith M, Fairley M, Johnson PDR. Acute, oedematous
Mycobacterium ulcerans infection in a farmer from far north Queensland.
Med J Aust 2002; 176: 180-181.
• Johnson PDR, Veitch MGK, Leslie DE, Flood PE, Hayman JA. The emergence of
Mycobacterium ulcerans infection near Melbourne. Med J Aust. 1996;164:76–8. [PubMed]
• Johnson PDR, Azuolas J, Lavender CJ, Wishart E, Stinear TP, et al. Mycobacterium ulcerans in mosquitoes captured during an outbreak of Buruli ulcer, southeastern Australia. Emerging Infective Diseases. 2007;13:1653–1660. [PubMed]
• Johnson P, Lavender C. Correlation between Buruli ulcer and vector-borne notifiable diseases, Victoria, Australia. Emerg Infect Dis. 2009;15:614–615. [PMC free article] [PubMed]
• Lavender C, Senanayake S, Fyfe J, Buntine J, Globan M, et al. First case of Mycobacterium ulcerans disease (Bairnsdale or Buruli ulcer) acquired in New South Wales. Med J Aust. 2007;186:62–63. [PubMed]
• Marsollier L, Robert R, Aubry J, Saint Andre J, Kouakou H, et al. Aquatic insects as a vector for Mycobacterium ulcerans. Appl Environ Microbiol. 2002;68:4623–4628. [PMC free article] [PubMed]
• Radford AJ. Mycobacterium ulcerans in Australia. Aust N Z J Med. 1975;5:162–9.
• Steffen CM, Smith M, McBride WJ. Mycobacterium ulcerans infection in North Queensland: the 'Daintree ulcer'. ANZ J Surg. 2010;80:732–736. [PubMed]
• Veitch MG, Johnson PD, Flood PE, Leslie DE, Street AC, Hayman JA. A large
localized outbreak of Mycobacterium ulcerans infection on a temperate southern
Australian island. Epidemiol Infect. 1997;119:313–8.[PubMed]
• Mycobacterium ulcerans Treatment Costs, Australia http://wwwnc.cdc.gov/eid/article/10/6/03-0428_article.htm
• Consensus recommendations for the diagnosis, treatment and control of Mycobacterium ulcerans infection (Bairnsdale or Buruli ulcer) in Victoria, Australia http://www.mja.com.au/public/issues/186_02_150107/joh10634_fm.html
Flesh-eating ulcer bacteria in Australia. ( 15 pages )
by Romsey Australia is licensed under a Creative Commons Attribution 2.5 Australia License.

Revised 16/04/2018